- by Alison
Dengue in the USA: Avoiding larger outbreaks and the wider spread of vector-borne disease
Dengue in the USA is mainly confined to its overseas territories, Puerto Rico and American Samoa in particular. The US mainland does, however, occasionally experience dengue outbreaks in its more subtropical parts – including Florida and the Gulf of Mexico. What more needs to be done to minimize the risk of dengue in the USA? We spoke with Dr. Ronald Rosenberg, Associate Director for Science at the Division of Vector-Borne Diseases, Centers for Disease Control and Prevention (CDC) and lead author of Vital Signs: Trends in Reported Vector-borne Disease Cases – United States and Territories, 2004–2016.
Dengue’s primary vector, Aedes aegypti, is established across large parts of the US, both in the overseas territories and the mainland. Despite this, the US mainland is largely free of dengue. Occasional outbreaks linked to imported cases from endemic countries typically infect fewer than 50 people.
It’s easy to see how dengue reaches the regions where outbreaks occur. In southern Texas and the other states bordering Mexico, for instance, large numbers of people travel back and forth across the border, providing “many opportunities for introducing dengue,” according to Dr. Rosenberg. Meanwhile, southern Florida, especially Miami, is an enormous air hub for Latin America and the Caribbean, “so we have large numbers of people traveling to and from places where dengue is endemic,” he adds.
DYK? Mosquitoes are the deadliest animal in the world. It only takes one bite from a mosquito to make you sick, but it takes a community to control mosquitoes. https://t.co/OuhqCJ7KG2 #CDC #MosquitoControl @CDC_NCEZID pic.twitter.com/ayJ3tLSTEU
— CDC (@CDCgov) July 2, 2018
The picture is very different in some of the US territories. “Puerto Rico is our main concern when it comes to dengue,” says Dr. Rosenberg. “All four dengue viruses, as well as chikungunya and Zika, are endemic.”
Reducing risks of dengue in the USA
We asked Dr. Rosenberg whether he expects outbreaks of dengue in the USA to increase on the mainland. He foresees some transmission to continue in areas that have already seen outbreaks but is very concerned that future outbreaks could be larger: “If weeks go by without a dengue outbreak being detected, we could have an epidemic in mainland US. Thus far, local authorities have identified them pretty rapidly.”
Florida, Texas and other places susceptible to dengue introduction have excellent dengue surveillance and vector control operations. “They have a lot of nuisance mosquitoes and good nuisance mosquito surveillance and control operations, which also control vector mosquitoes,” says to Dr. Rosenberg.
Other parts of the US, he feels, need better surveillance and “badly need better vector control”, which is “too fragmented”. In the US, vector control departments exist at city or county level, not often at the state level. “Vector control operations in one town could be really good, but then a nearby town may have no vector control operations at all,” says Dr. Rosenberg.
Networking operations
To increase communications, enhance information sharing and develop best practices, the CDC is building a network of vector control officials. Dr. Rosenberg would like to see this network be as good as the US’s excellent network of state laboratories, which is very effective in diagnosing cases of dengue and other diseases. Every lab in the US’s Laboratory Response Network is kept up to date with the best tests needed to detect dengue, or another disease, outbreak.
On the surveillance side, the CDC is mapping Aedes aegypti, along with Aedes albopictus, populations with the help of the network it’s building. “During the 2016 Zika outbreak, we found many mosquito operations didn’t know they had Aedes aegypti in their area,” says Dr. Rosenberg. “We asked them to look for where Aedes aegypti can actually be found. We then built on that by modeling where we think it could be found.”
The CDC used that information to build and publish maps of the potential range of Aedes aegypti and Aedes albopictus populations in the US:
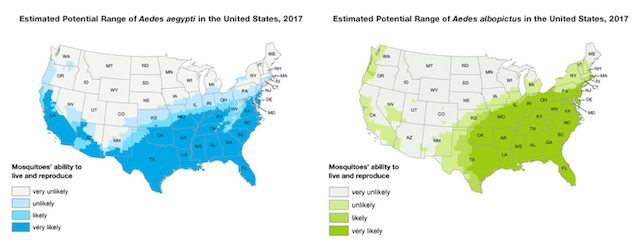
Nevertheless, Dr. Rosenberg would still like to know more precisely where Aedes aegypti is. “We will continue monitoring so we know if it’s spreading,” he says.
Improving know-how
The CDC is also providing training to ensure those involved in dengue surveillance and control have a good understanding of Aedes aegypti and how to respond if there is a disease outbreak.
Take insecticide resistance, for instance; it’s a big problem in the US and significantly hinders vector-borne disease control efforts. Again, during the Zika outbreak, the CDC found many US mosquito control operations had never done any insecticide testing. “If there’s an outbreak of disease and vector control operations spray areas where the mosquitoes are resistant to the insecticide, they’re wasting time and money – and not controlling the outbreak,” says Dr. Rosenberg.
The CDC is now working with mosquito control organizations to build a robust network of well-trained mosquito control operatives who can test for insecticide resistance. “We want them to have the equipment and strategies for responding to an outbreak, or even just to suppress Aedes aegypti populations as a preventative measure,” says Dr. Rosenberg.
The network is also improving operatives’ public relations skills because, as Dr. Rosenberg points out, “Aedes aegypti breeds around people’s houses and containers, so you need the community to help with depriving it of a place to reproduce”.
More research needed
Dr. Rosenberg agrees that the US needs better tools for suppressing Aedes aegypti: “There are more innovative methods on the horizon. We’d certainly like to see more results from the various sterile insect technique releases like Wolbachia bacteria and irradiated males, or the RIDL(Release of Insects carrying Dominant Lethals) technique.”
Why should you care about #MosquitoControl? Since 1999, epidemics like #WestNileVirus, #dengue, #chikungunya, #Zika, happen more. State & local government agencies must be able to prevent and control. @EntsocAmerica @NACCHOalerts @305Mosquito pic.twitter.com/vj9nbKqQAT
— CDC Emerging Infections (@CDC_NCEZID) June 26, 2018
He would also like to see more research on epidemiology modeling. He nevertheless acknowledges that the dynamics of the transmission of vector-borne diseases are very difficult to model: “You don’t know with much certainty where the mosquito is going and how far it will fly, and you don’t know if it’s going to bite somebody who has dengue.”
While models could be very helpful, they are always limited by the accuracy and the completeness of the information put into them. “Responding to an outbreak requires precise models, and that requires more research into the biology and habits of Aedes aegypti,” he says.
Finally, Dr. Rosenberg shares his thoughts on how dengue in the USA is intimately linked to the global dengue problem. “We’re not going to remove the threat of dengue in the USA, even if it is limited until we reduce dengue transmission in Latin America, South East Asia, and Africa,” he says. “After all, you can get on an airplane any place in the world feeling perfectly fine, then get off the airplane with dengue having been bitten by a mosquito.”
Is low-cost travel spurring dengue outbreaks?
—
Reduce the impact of dengue near you. Report local dengue fever activity using Dengue Track.

